 Methicillin-resistant Staphylococcus aureus (MRSA) infection
Methicillin-resistant Staphylococcus aureus (MRSA) infection Written by Dr Alan Johnson, clinical scientist
What is MRSA?
Staphylococcus aureus is a species of bacterium commonly found on the skin and/or in the noses of healthy people. Although it is usually harmless at these sites, it may occasionally get into the body (eg through breaks in the skin such as abrasions, cuts, wounds, surgical incisions or indwelling catheters) and cause infections. These infections may be mild (eg pimples or boils) or serious (eg infection of the bloodstream, bones or joints).
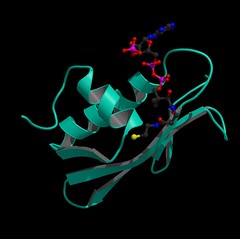
MRSA stands for methicillin-resistant Staphylococcus aureus, which is a type of Staphylococcus aureus that is resistant to the antibacterial activity of methicillin and other related antibiotics of the penicillin class.
The treatment of infections due to Staphylococcus aureus was revolutionised in the 1940s by the introduction of the antibiotic penicillin.
However,, most strains of Staphylococcus aureus are now resistant to penicillin. This is because Staphylococcus aureus can make a substance called ß-lactamase (pronounced beta-lactamase), that degrades penicillin, destroying its antibacterial activity.
In the early 1960s, a new type of penicillin antibiotic called methicillin was developed. Methicillin was not degraded by ß-lactamase and so could be used to treat infections due to ß-lactamase-producing strains of Staphylococcus aureus. Subsequently, methicillin was replaced by newer and better penicillin-type antibiotics (such as flucloxacillin) that were also not affected by ß-lactamase.
Unfortunately, shortly after the introduction of methicillin, certain strains of Staphylococcus aureus emerged that were resistant to methicillin (and also to the newer drugs such as flucloxacillin) These methicillin-resistant Staphylococcus aureus became known as 'MRSA' for short, and although methicillin is no longer prescribed, having been replaced by flucloxacillin, the term MRSA continues to be used.
Although other types of antibiotics can still be used to treat infections caused by MRSA, these alternative drugs are mostly not available in tablet form and must be administered through a drip inserted into a vein or by injection.
MRSA infections in hospital
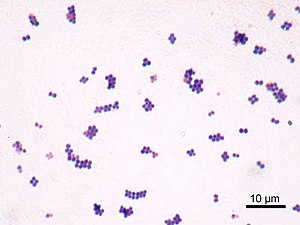 Image via Wikipedia
Image via WikipediaMRSA infections are a particular problem in hospitals. As with ordinary strains of Staphylococcus aureus, some patients harbour MRSA on their skin or nose without harm (such patients are said to be 'colonised'). However, these patients may develop infections if the MRSA spread to other parts of the body (eg if MRSA spread from the colonised nose to a wound). When this happens the resulting infection is described as 'endogenous'.
Some patients are at increased risk of developing infection. They include those with breaks in their skin due to wounds or indwelling catheters which allow MRSA to enter the body, and those with certain types of deficiency in their immune system, such as low numbers of white cells in their blood.
Individuals colonised with MRSA may also serve as a 'reservoir' of MRSA that may spread to other patients. This may happen, for example, if hospital staff attending to a colonised or infected patient become contaminated or colonised with MRSA themselves (often only briefly) and spread the bacteria to other patients with whom they subsequently have contact. These patients may in turn become colonised and/or infected. The spread of MRSA (or for that matter other bacteria) between patients is called cross-infection. In addition, MRSA may be spread via contaminated equipment or through the environment.
Some strains of MRSA are particularly successful at spreading between patients and may also spread between hospitals, presumably when colonised patients or staff move from one hospital to another. These strains are known as epidemic MRSA (or EMRSA for short). During the 1990s there was a marked increase in infections caused by MRSA in hospitals in the UK due to the emergence and spread of two particular stains of EMRSA known as EMRSA-15 and EMRSA-16.
MRSA infections in the community
 Image by AJC1 via Flickr
Image by AJC1 via FlickrPatients may be colonised with MRSA when they leave hospital, and there has long been concern that MRSA might spread from hospitals into the community.
In recent years increasing numbers of cases of MRSA infection in the community have been seen in many countries around the world, particularly the USA. However, investigations of these cases have shown that in many instances, the strains of MRSA found in patients in the community are distinct from those strains seen in hospitals and it now appears that these so called 'community-associated MRSA' have evolved independently of hospital MRSA. Although infections with 'community-associated MRSA' occur frequently in some countries, they are uncommon in the UK.
Studies in the USA and other countries have shown that the 'community-associated MRSA' often cause infections in previously healthy individuals who lack the risk factors seen in hospitalised patients. Many of these strains have a toxin called the Panton-Valentine leucocidin (usually referred to as 'PVL') which may contribute to their increased ability to cause infections.
Luckily, 'community-associated MRSA' are frequently susceptibility to a wide range of antibiotics (apart from those belonging to the penicillin class). As further evidence of their independent evolution, 'community-associated MRSA' are generally susceptible to a wider range of antibiotics than are hospital strains.
Can the spread of MRSA be controlled?
 Image by estherase via Flickr
Image by estherase via FlickrThere are several steps that may be undertaken to minimise the spread of MRSA between patients.
Hospital staff should wash their hands scrupulously before and after having physical contact with patients, using soap or rapidly acting antibacterial alcohol solutions.
Patients colonised or infected with MRSA may be kept away from other patients by being placed in separate rooms, either alone or with other patients who also have MRSA. Access to such rooms should be restricted to essential personnel.
Hospital staff should wear gloves and disposable gowns prior to having physical contact with MRSA patients. Before leaving the room, they should discard these safely, and wash their hands.
Visitors and carers likely to have a lot of physical contact with patients should also wear disposable gloves and gowns. All visitors should wash their hands before leaving the room.
MRSA can survive on inanimate objects or surfaces such as linen, sinks, floors and even mops used for cleaning. For this reason, areas where MRSA patients are nursed should be thoroughly cleaned using disinfectants.
How is infection or colonisation with MRSA diagnosed?
To diagnose MRSA infection, specimens such as a swab of an infected wound or a sample of blood are taken from the patient. These are sent to a microbiology laboratory, where bacteria present in the specimen are cultured and identified. This process may take several days.
In addition, sometimes more rapid tests which detect the DNA (the genetic material) typically found in MRSA may be undertaken. Colonisation with MRSA is detected similarly, using swabs of a person's skin or from the inside of the nose.
How is MRSA treated?
 Image by AJC1 via Flickr
Image by AJC1 via FlickrPatients colonised with MRSA may have a special antibiotic called mupirocin applied onto their skin (Bactroban) or the inside of their nose (Bactroban nasal). This helps to eliminate the MRSA and reduces the risk of the bacteria spreading either to other sites on the patient's body, where they might cause infection, or to other patients. Some strains of MRSA are, however, resistant to mupirocin.
Individuals colonised with MRSA may also wash their skin and hair with suitable disinfectants, such as chlorhexidine.
Patients infected with MRSA
 Image by AJC1 via Flickr
Image by AJC1 via FlickrAlthough MRSA are resistant to many drugs, most remain susceptible to the antibiotics vancomycin and teicoplanin (Targocid). Infections due to MRSA are therefore often treated with one or other of these drugs. Both must be administered by infusion or injection, and for this reason, they are used for treatment only in hospitalised patients. Injection of vancomycin into muscle is painful and thus not used, while rapid administration into a vein may produce an allergic-type reaction (the so-called 'red man' syndrome). To overcome these problems, vancomycin must be given by slow infusion into a vein. In contrast, teicoplanin may be safely administered by injection into muscle or rapid infusion into a vein.
A very few MRSA resistant to vancomycin and/or teicoplanin have been found in the USA and although there is concern that they may become more common, there is no evidence of this happening to date. Fortunately, in the last few years further antibiotics that are active against MRSA have been developed and licensed for clinical use.
One such drug, called linezolid (Zyvox) may be given either by intravenous infusion (in severely ill patients) or in tablet form. Clinical trials have so far shown it is useful (either alone or in combination with other antibiotics) for the treatment of pneumonia and skin and soft tissue infections.
More recently, another drug called daptomycin (Cubicin) has been licensed for the treatment of skin, soft tissue, heart and blood infections including those caused by MRSA.

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.