Wikinvest-Seattle Genetics (SGEN)
Disappointing news reported from Seattle Genetics today. I actually like the stock after the price bottoms out as they are focusing their efforts on Non-Hodgkins Lymphoma drug, brentuximab. Wait for the massive sell-off in the next week or two and wait for Clinical Trials results to come out in about 6 weeks from Phase II testing for NHL. I anticipate a massive sell-off in the next couple of days after todays disappointing clinical trials news on a separate medication for AML, acute myeloid leukemia.
KEYWORDS: Antibody-Drug Conjugates, Millenium Pharmaceuticals, Seattle Genetics, AML, Monoclonal Antibody Therapeutics, Hodgkin Lymphoma
Seattle Genetics is ditching further development of its clinical-stage acute myeloid leukemia (AML) candidate lintuzumab (SGN-33) after a Phase IIb trial failed to show the drug extended overall survival. The firm says it will now focus on the rest of its clinical pipeline, headed by the Phase III-stage Hodgkin lymphoma drug, brentuximab vedotin, which is being developed in collaboration with Millennium Pharmaceuticals.
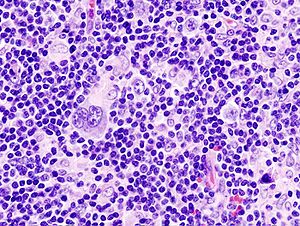
Lintuzumab is a naked mAb targeting CD33. The Phase IIb study evaluated the drug in combination with low-dose cytarabine chemotherapy in 211 previously untreated AML patients aged 60 years or older who were ineligible for or declined intensive chemotherapy. Seattle said it was “disappointed” that the trial failed to show an overall survival benefit associated with lintuzuab in this older patient population.
Seattle’s lead candidate, brentuximab vedotin, is an antibody-drug conjugate comprising an anti-CD30 monoclonal antibody linked to monomethyl auristatin E (MMAE). Top-line data from a pivotal study evaluating brentuximab vedotin in patients with relapsed or refractory Hodgkin lymphoma is under way under a Special Protocol Assessment with the FDA at multiple sites in North America and Europe. The firm says top-line data from the trial is expected within the next six weeks, and a regulatory submission could be filed within the first half of 2011. A Phase II clinical trial evaluating brentuximab vedotin in patients with relapsed or refractory systemic anaplastic large cell lymphoma (ALCL) is also due to report interim top-line data within the next six weeks. Seattle hopes systemic ALCL may provide an additional registration pathway for the drug. Meanwhile, in May the firm and its partner, Millennium, initiated a Phase III trial (designated Aethera) to investigate brentuximab vedotin in the treatment of patients at high risk of residual Hodgkin lymphoma following autologous stem cell transplant.
The firms inked their worldwide agreement to develop brentuximab vedotin during December 2009. Under the terms of the agreement, Seattle Genetics and Millennium's parent company, Takeda Group, are sharing worldwide development costs on a 50:50 basis. Seattle received an up-front payment of $60 million, and retains full commercialization rights to brentuxiamb vedotin in the U.S. and Canada. Takeda has exclusive rights to commercialize the product in all other countries in return for development and sales milestone payments, which Seattle says could reach over $230 million.
Seattle's clinical pipeline also includes antibody-drug conjugates and an engineered monoclonal antibody in Phase I trials. Dacetuzumab (SGN-40) is a humanized mAb targeting the CD40 antigen and is currently undergoing four Phase Ib clinical trials as combination therapy against non-Hodgkin lymphoma and multiple myeloma.
SGN-70 is a humanized anti-CD70 mAb in a Phase I trial in patients with autoimmune disease, and SGN-75 is a humanized anti-CD70 mAb attached to the synthetic drug payload, monomethyl auristatin F (MMAF). Developed using Seattle’s antibody-drug conjugate (ADC) technology, SGN-75 is currently undergoing a Phase I clinical trial in patients with relapsed or refractory non-Hodgkin lymphoma or metastatic renal cell carcinoma.
ASG-5ME is an antibody-drug conjugate comprising a fully human monoclonal antibody targeting the anticancer target SLC44A4 (AGS-5), attached to monomethyl auristatin E (MMAE) via an enzyme-cleavable linker designed to release the cytotoxic agent only once it has been delivered to antigen-expressing cancer cells. A single-agent, open label dose-escalation trial evaluating the safety, tolerability, pharmacokinetics, and antitumor activity of ASG-5ME is under way in patients with metastatic pancreatic cancer.
Antibody-Drug Conjugates to Fight Cancer
B-cell lymphoma has gotten plenty of attention from drug developers. Some spectacularly successful drugs, particularly mAbs, have improved its treatment and prognosis. Rituxan, arguably the biggest game-changer in non-Hodgkin B-cell lymphoma treatment, targets the CD20 antigen present on B cells. But a different antigen altogether, CD30, characterizes Hodgkin lymphoma (HL). HL has historically been considered curable with radiation and chemotherapy.
Why, then, is Seattle Genetics collaborating with Millennium Pharmaceuticals: The Takeda Oncology Company to develop brentuximab vedotin, an antibody drug conjugated (ADC) chemotherapeutic to treat HL? The market is relatively tiny compared to non-Hodgkin B-cell lymphoma, with an annual incidence of about 8,500 (as of 2009) in contrast to B-cell lymphomas, which generally occur in individuals older than 50, with an annual incidence of 65,980 (as of 2009). Additionally, patients diagnosed with HL during 2006–2010 had long-term survival expectations close to or exceeding 90% in all age groups up to age 45. Survival rates exceeded 80% and 70% in the 45–54 and 55–64 age groups, respectively.
But, Clay Siegall, M.D., Seattle Genetics’ president and CEO, pointed out to GEN, “We have plenty of patients to treat, and HL isn’t a cured disease.” Seattle Genetics is also targeting T-cell lymphomas, a group of malignancies that also express the CD30 antigen. The company believes that ADCs have the potential to offer safer options.
Rationale for Using ADCs in HL
Despite high cure rates and low incidence, HL presents a unique opportunity as a target for ADC-based therapy. Hodgkin remains the most common malignancy in people between 10 and 30 years of age; the average age at which it occurs is about 28. This means that the majority of individuals who get HL are young, with potentially long lives ahead of them.
The disease has generally been treated with the chemotherapy regimen ABVD (adriamycin, bleomycin, vinblastine, dicarbazine) and, until recently, with radiation to treat refractory or relapsed disease. Young children were routinely treated with radiation delivered to multiple body sites to achieve remissions. These so-called cures, however, were achieved at considerable cost to some patients whose long-term survival was compromised by the development of other serious illnesses.
And apart from the need for better and safer treatment methods for younger patients, Dr. Siegall noted that “when we looked at HL and talked to experts in the disease, 25% of all HL patients are treatment-refractory or relapse, so we saw an unmet need.”
In 2008, researchers at Stanford University reported that low-dose radiation for HL leaves children at a significant risk for second malignancies. And a study published in 2009 revealed that women who had been treated during childhood with radiation for HL were almost 40 times more likely than others to develop breast cancer. Also, HL patients treated with radiation have a substantially higher risk of stroke, according to a study published in 2009 in the Journal of the National Cancer Institute (JNCI).
In an editorial accompanying the JNCI report, the National Institute of Aging’s Dan Longo, M.D., commented that the findings added to the already overwhelming evidence that using radiation therapy in HL was shortsighted. “Although treatments for this disease have included reduced doses of radiation since 1995, there is no evidence yet that this translates into fewer late effects for survivors.”
By empowering antibodies by linking them to chemotherapeutic agents, Seattle Genetics and other companies hope they will provide a novel form of therapy for HL and improve treatments for other cancers. ADCs are considered attractive, safer alternatives to conventional chemotherapy because they combine the specificity of mAbs with the potency of cytotoxic molecules, delivering them directly to their intended targets and, theoretically, avoiding systemic toxicity.
Seattle Genetic’s brentuximab vedotin combines an anti-CD30 antibody linked to its synthetic drug payload, monomethyl auristatin E, an antitubulin. Like other ADCs, the antibody/cytotoxin construct is designed to be stable in the bloodstream but to release the cytotoxic drug upon internalization into CD30-expressing tumor cells. Seattle Genetics notes that its technology allows stable linkage of the antibody to a chemotherapeutic agent. It has been licensed by several companies including Bayer Healthcare, CuraGen, and Progenics to develop new cancer therapies.
The CD30 antigen, according to Seattle Genetics, provides an attractive target for cancer therapy because it is expressed on Hodgkin lymphoma, several types of T-cell lymphomas, and other hematologic malignancies but has limited expression on normal tissues.
Seattle Genetics and Millennium reported in February that they have initiated a Phase I trial of brentuximab vedotin in combination with chemotherapy for the treatment of newly diagnosed HL patients. “We are on track to report top-line data from our pivotal brentuximab vedotin trial for Hodgkin lymphoma in the second half of 2010, positioning us for a planned New Drug Application submission in the first half of 2011,” Dr. Siegall said.
Technology Shows Potential to Expand into Other Cancers
ADC technology also has the potential to extend the use of currently marketed antibodies. ImmunoGen says that its payload technology, which is used in the only armed antibody, Herceptin, has shown activity in patients whose cancer progressed on the same, unmodified antibody. TDM1 is a conjugate of the chemotherapy agent DM1 and the Herceptin antibody. DM1 belongs to the maytansine class of chemotherapies that targets microtubules.
Roche (RHHBY) and Genentech reported results of a clinical trial of TDM1 in December 2009, showing that it shrank tumors in women with highly advanced Her-2 positive breast cancer. Women in the study had already been treated with an average of seven drugs for metastatic disease prior to receiving the ADC, including chemotherapy, Herceptin, and Tykerb (GlaxoSmithKline-GSK).
“Despite major advances in Her2-positive breast cancer, the disease may still progress after multiple treatments, to the point where there are no approved Her2-targeted medicines,” Hal Baron, M.D., evp of global development and CMO at Roche, noted. “Results from this study are promising for women who need new treatment options, and we will discuss the next steps of the TDM1 development program with the FDA.”
Following the Rituxan model, Seattle Genetics is focused on getting its first FDA approval for relapsed HL and for anaplastic large-cell lymphoma and then combining it with chemotherapy for first-line HL treatment. “Ultimately,” Dr. Siegall commented, “in HL we have a great opportunity to bring the drug to the front line to get a higher percentage of patients with durable complete responses, lessen the amount of chemotherapy, and, maybe, get rid of the radiation therapy.
“Monoclonal antibodies are phenomenal drugs,” Dr. Siegall said but added that empowered ADCs will provide the next generation of blockbuster antibodies.

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.