 Image via Wikipedia From the NY Times
Image via Wikipedia From the NY TimesBy GINA KOLATA
Published: July 16, 2010
Marilyn Maldonado is not quite sure why she is at the Memory Enhancement Center in the seaside town of Oakhurst, N.J.
“What are we waiting for?” she asks. About 10 minutes later, she asks again. Then she asks again.
She is waiting to enter a new type of Alzheimer’s drug study that will, in the boldest effort yet, test the leading hypothesis about how to slow or stop this terrifying brain disease.
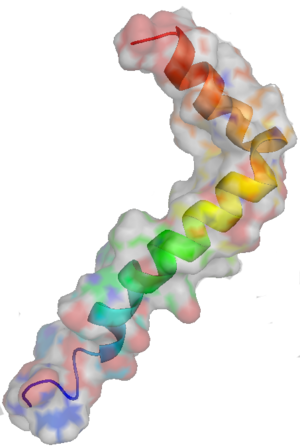
The disease is defined by freckles of barnacle-like piles of a protein fragment, amyloid beta, in the brain. So, the current thinking goes, if you block amyloid formation or get rid of amyloid accumulations — plaque — and if you start treatment before the disease is well under way, you might have a chance to alter its course.
On Tuesday, that plan got a new push. The National Institute on Aging and the Alzheimer’s Association proposed new guidelines for diagnosis to find signs of Alzheimer’s in people who do not yet have severe symptoms, or even any symptoms at all.
The guidelines are needed for the new approach to Alzheimer’s drug development. Just about every pharmaceutical company and many biotechnology companies have experimental drugs to block amyloid — there are more than 100 in the pipeline. And the companies would like to show that if they give their drugs early, they can slow or stop the disease.
That is the ultimate goal for the drug in the study Mrs. Maldonado wants to enter, sponsored by Bristol-Myers Squibb. The company is, for the first time, testing such a drug in patients who, on evaluation with memory tests and new brain scans and tests for amyloid in cerebrospinal fluid, seem to be in a very early stage of Alzheimer’s. The idea is to attack the disease when there may still be time to stop the worst brain cell death.
But there is a problem. The Food and Drug Administration says it needs to know not just that plaque was reduced or even that it disappeared, but that those who took a drug ended up with better memory and better ability to think and reason as compared with those who did not take the drug.
Alzheimer’s, though, progresses so slowly that showing that a drug, started early, affects symptoms can take far longer than companies can afford to wait.
There is reason not to accept other forms of proof, like scans or cerebrospinal fluid that show changes in amyloid in the brain, the F.D.A. says. The agency has approved drugs for diseases, including sudden death from heart arrhythmias, on the basis of tests that showed symptoms, like heart rhythms, improved. Then it turned out the drugs did not affect the course of the disease and, in the case of the heart drugs, actually hastened death.
So the Alzheimer’s field is poised at an agonizing point — ready to move forward with new methods of diagnosis and drugs that might modify the course of the disease, but without proof that blocking amyloid actually makes a difference.
In the meantime. Bristol-Myers is trying a two-pronged strategy to gain faster approval. It is starting treatment early, but not so early that patients are a decade or more away from Alzheimer’s. And as it looks for effects on symptoms like memory and reasoning, the company will be tracking what happens to amyloid in the brain, hoping to show symptoms improve or no longer worsen as plaque formation slows or stops.
It is a gamble for the company, because even people with fairly mild symptoms may have too much brain damage to be helped. But it is a strategy that makes sense, said Dr. Dennis J. Selkoe, a Harvard researcher who is not affiliated with the study.
“In my view, the sweet spot for amyloid-lowering trials is mild Alzheimer’s disease,” Dr. Selkoe said. “As soon as one of those trials shows benefit, everyone will move to prevention trials,” he said. “They will begin treating before there are symptoms.”
Mrs. Maldonado may be one of the pioneers.
The Amyloid Hypothesis
Considering how important a medical problem Alzheimer’s is — afflicting 5.3 million Americans, the seventh-leading cause of death, and devastating and bankrupting families — it took a surprisingly long time to be recognized as a disease at all. And it took longer still to reach any kind of agreement on its cause.
Dr. Paul Aisen, an Alzheimer’s expert at the University of California, San Diego, remembers well the old days, in the late 1970s. He was in medical school, studying to be a geriatrician. There was no discussion of Alzheimer’s disease.
Ever since it was described by Dr. Alois Alzheimer in 1906 as a “peculiar” disease in a 51-year-old woman, doctors had considered it an oddity, a rare illness of middle, not old, age. Old people who lost their memory and ability to reason and care for themselves were said to be “senile.” That word did not refer to any specific disease like Alzheimer’s. Senility, Dr. Aisen said, was “what might happen when you got old.” And “there was nothing you could do about it.”
Then, in 1976, doctors’ eyes were opened by an editorial in Archives of Neurology by Dr. Robert Katzman, a neurologist. Alzheimer’s, he wrote, is not rare — it is common. It can arise in old age. And it is a leading cause of death and, Dr. Katzman said, a disease whose origin could be determined and whose course might be stopped.
Neurologists took note. But it was 20 years before there were any drugs for Alzheimer’s, and the four approved so far treat only symptoms, modestly and temporarily improving memory, for example, and do not affect the relentless brain cell death.
In the meantime, researchers came upon an exciting target for a drug. They discovered two enzymes that snip pieces from a large protein protruding from brain cells. The result is toxic fragments of a substance known as amyloid beta peptides. Those shards accumulate as plaques on the brain. One way to prevent plaques might be to block one of those crucial enzymes.
Just about every drug company got to work.
They had long suspected amyloid beta was a key player in the genesis of Alzheimer’s, but until they found the enzymes researchers had no way to block it. Amyloid beta itself might be injuring nerve cells or the plaques, made of accumulations of amyloid beta, could be the culprits. But whichever was true, three lines of evidence pointed to amyloid beta: rare gene mutations that lead to its overproduction cause Alzheimer’s in middle age. Down syndrome also causes overproduction of amyloid beta, and people with Down always get Alzheimer’s. And when scientists put the rare mutated genes that cause Alzheimer’s into mice, the mice developed plaques and memory problems.
The logic was not airtight. Scientists note that older people with typical Alzheimer’s often have something else wrong in their brain — damage from mini-strokes, for example. Perhaps some of these other conditions set off waves of cell death independent of amyloid beta.
But over the years, researchers say, what has become known as the amyloid hypothesis — the notion that overproduction or reduced clearance of amyloid beta is a cause of the disease and blocking amyloid beta could stop it — dominated their thinking.
“Ninety percent of us in the field believe it is correct,” Dr. Aisen said.
An Antibody Approach
Testing of the amyloid hypothesis began a few years ago with two experimental anti-amyloid drugs, homotaurine and tarenflurbil.
Patients who took them did not improve.
But, some researchers asked, was that a fair test? The first drug was not very potent, and little of the second reached the brain. And it was not clear whether either was really affecting amyloid because there were no direct measurements of plaques or amyloid beta protein.
The results, said Dr. Samuel E. Gandy, a professor of Alzheimer’s disease research at Mount Sinai School of Medicine, were “uninterpretable.”
Then there was the vaccine approach — immunize against amyloid beta and let the immune system clear plaque. It worked in mice and so, to great excitement, researchers tested it in patients. But a preliminary study was abruptly halted when 18 of 300 patients developed a brain inflammation. Two immunized patients who later died after reaching “severe end-stage dementia” had almost no plaque in their brains on autopsy — the vaccine had apparently cleared plaques but not noticeably affected their disease.
But that is not proof a vaccine would not work, said Dr. Selkoe, a founder of the company that did the study and a consultant to it. Two patients hardly constitutes a full analysis of the trial data, he says.
Now, the company, Elan, and its collaborators are trying a different tack. Instead of using a vaccine, they made an antibody to amyloid beta, a drug called bapineuzumab.
Some initial results were published in March. A new type of scan that can show plaques found the drug was removing them. But so far it is unclear whether patients are improving.
Johnson & Johnson, which partnered with Elan and its collaborator, Pfizer, says it will continue the study.
That makes sense, said Dr. Gandy, who is not part of the study.
“We have no idea how long we might need to treat,” he said.
Tough Road to Consensus
Dr. Russell Katz, director of the F.D.A.’s division of neurology products, is in a quandary about Alzheimer’s drugs. What, he must decide, should be the criteria for showing that a drug works?
Should the F.D.A. say it is sufficient to show that a treatment prevents or lessens the formation of plaque?
The agency is not ready to do that, Dr. Katz said.
“You only care if down the road the patient gets better,” Dr. Katz said. “What we are concerned about is approving a drug based on a lab test and being wrong about what happens to the patient clinically.”
With Alzheimer’s, Dr. Katz said, “the great fear is that maybe amyloid has nothing to do with the disease.” If that were the case, and the agency approved a drug that blocked amyloid formation, millions of healthy people could end up taking something useless or even dangerous. And because it takes so long for Alzheimer’s to develop, it could be decades, if ever, before anyone knew the drug did not work.
“It is a conundrum,” Dr. Katz said. “We all hope to get to the point in our understanding of the disease process where everyone in the field says: ‘Look. We know it now. Amyloid causes Alzheimer’s, and we have drugs that decrease amyloid.’ But we are not there yet.”
Bristol-Myers Squibb, though, is betting amyloid beta is the culprit. And it is betting it can show an effect in people who are in the early stages of Alzheimer’s.
Still, Dr. Aisen is concerned that even those patients, people like Mrs. Maldonado, might be beyond help. Treatment may have to start much earlier. So he is planning a large federal study to test amyloid-blocking drugs in people over 70 with normal memories but evidence of some amyloid accumulation. His criteria for success will not be the F.D.A.’s current one. Instead, he will ask whether the drugs slow the brain atrophy that is characteristic of Alzheimer’s and prevent amyloid from accumulating in subjects’ brains.
“If you think Bristol-Myers Squibb is going out on a limb, this is going farther,” Dr. Aisen said. If blocking amyloid beta and slowing brain atrophy are not accepted as sufficient evidence that a drug works, a study with normal 70-year-olds could end up taking 10 to 15 years to show an effect on the actual symptoms of Alzheimer’s.
After her scan that recent day, Mrs. Maldonado was entered in the Bristol-Myers study.
She is 82, a former school bus driver living in nearby Jackson with a diagnosis of mild memory impairment. She came with her son-in-law to the Memory Center that day, in black slacks and a flowered blouse, wearing a gold bracelet and gold rings. Her short white hair was fluffy, freshly washed. And she had a way about her, a joking demeanor, intended to disguise her forgetfulness.
Her brain, the scan showed, was riddled with plaque.
Dr. Joel Ross, who runs the Memory Center, told her the results.
“We found you are producing a sticky material called plaque,” he told her.
“Yeah,” she said.
“It’s coating some of your brain.”
“Yeah,” she said again.
“If you stay this way there will be a lot of it.”
“Yeah.”
“So we’re going to give you a drug that may clear it up.”
“Yeah.”

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.